Arterial Services
Peripheral Artery Disease
Lower extremity Peripheral Artery Disease (P.A.D.) is a common disease that decreases the blood flow in the arteries to the legs and feet. P.A.D. can cause: leg muscle fatigue, discomfort or pain when walking; diminish quality of life and independence; and can lead to amputation. All people with P.A.D. have a two to six-fold higher risk of death from heart attack and stroke.
What Causes P.A.D.?
P.A.D. is caused by the build-up of fatty deposits (plaque) and cholesterol in the arteries outside the heart. These factors can increase your risk for P.A.D.:
Increasing age
Cigarette smoking
Diabetes
High Blood Pressure
Abnormal blood cholesterol
Personal history of heart attack or stroke
Signs and Symptoms of P.A.D.
Many people with Peripheral Artery Disease do not have any obvious symptoms. But others with P.A.D. may experience one or more of the following:
Leg muscle discomfort or pain that is consistently caused by walking and that disappears with rest. This symptom is called “claudication”.
Foot or toe pain at rest that often disturbs sleep
Skin wounds or ulcers on the feet or toes that heal slowly (don’t heal for 8-12 weeks)
Diagnosing Peripheral Artery Disease
Diagnosing P.A.D. is easy to diagnose and can be done through the following methods:
A medical history and physical examination of the feet and leg pulses
The ankle-brachial index (ABI), a test that compares the blood pressure in your ankles to that in your arms
Other studies, measuring the leg blood pressures (segmental pressure), toe pressures (toe-brachial index or TBI) or artery blood flow with ultrasound.
How to manage and treat Peripheral Artery Disease
If you smoke, set a quit date and ask for help to succeed.
Lower your blood pressure to less than 140/90 mmHg or to less than 130/80 mmHg if you have diabetes or chronic kidney disease
Lower your LDL (bad) cholesterol to less than 100mg/dL
If you have diabetes, manage your blood glucose and practice proper foot care
Use of antiplatelet medications to reduce your risk for heart attack and stroke
With Claudication
Exercise, preferably carried out in a supervised P.A.D. rehabilitation program, is an important treatment for reducing symptoms. Whether under supervision or on your own, the goal is to walk slowly, until you feel discomfort, rest and then walk again. Do this at least 35 minutes a day, at least three times a week. Gradually increase your time, distance, and endurance.
Certain medications may reduce your symptoms
Angioplasty, stenting, or surgical procedures may be effective options to reduce symptoms.
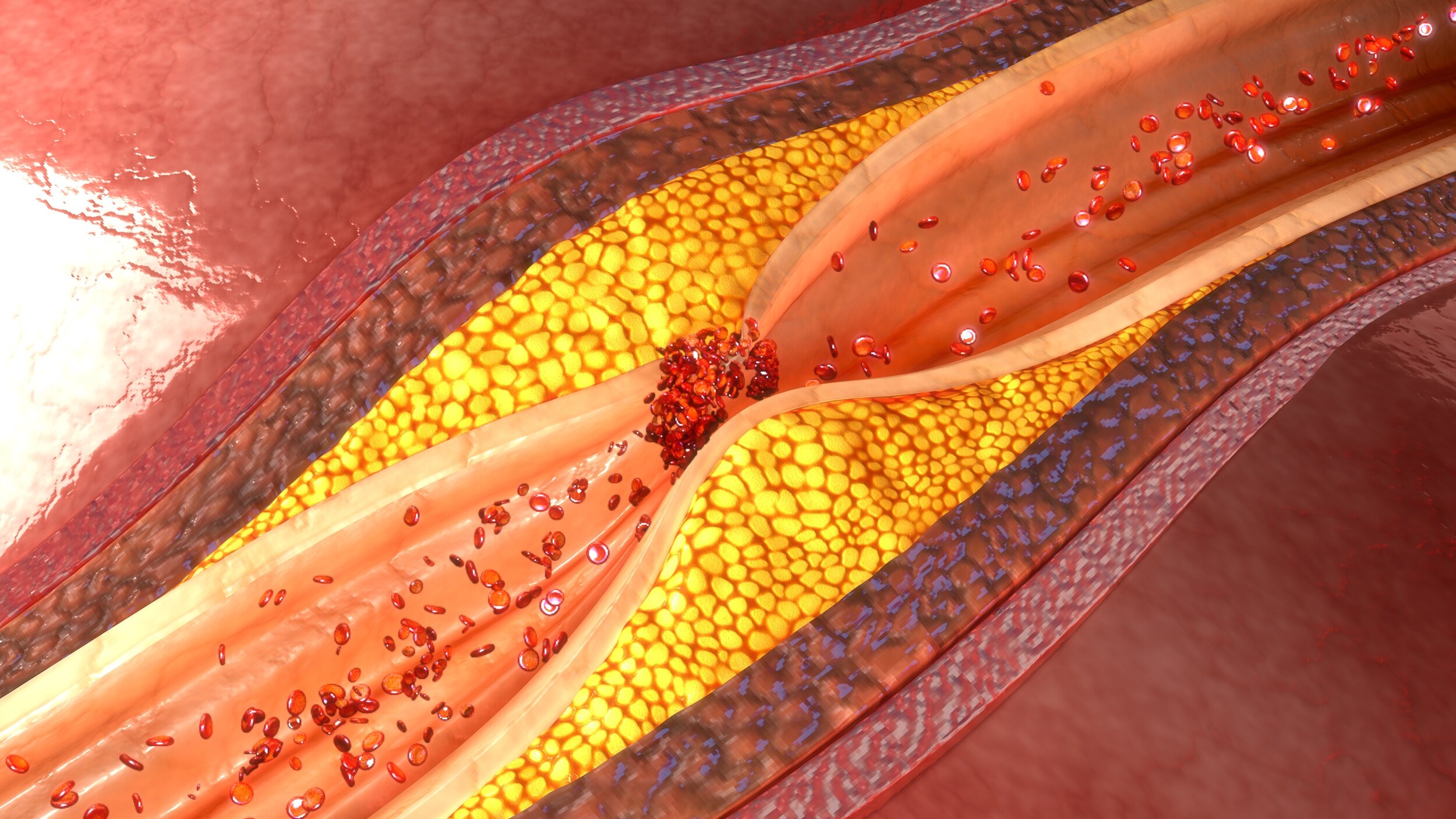
Atherosclerosis
Atherosclerosis refers to the build up of plaque (consisting of fat, cholesterol and other substances) within the arteries, which over time hardens and leads to reduced blood flow through the body. As arteries are the pathway for oxygen and nutrients to travel around the body, a blockage can lead to serious health issues, and if a plaque deposit bursts or a clot develops, this could lead to a heart attack, stroke or heart failure.
Commonly associated with the arteries surrounding the heart, atherosclerosis can occur anywhere in the body including the heart, brain, arms and legs (peripheral artery disease) and arteries leading to the kidneys. Particular attention should be taken for symptoms of inadequate blood flow including:
Chest pain (angina)
Pain or numbness in the leg or other limbs
Shortness of breath
Fatigue
Confusion
Muscle weakness.
A sign of atherosclerosis is painful cramps in the legs or backside when climbing stairs or exercising, due to reduced blood flow to the legs (intermittent claudication). Treatment for atherosclerosis can be through medications to reduce your cholesterol and manage other symptoms, or through surgical means such as bypass surgery, angioplasty, thrombolytic therapy or others. Angioplasty is a minimally invasive procedure that involves using a catheter to thread a balloon to the obstruction, where it is inflated to allow adequate blood flow through the artery. In some cases a metal stent will be placed to keep the artery open and prevent further narrowing.
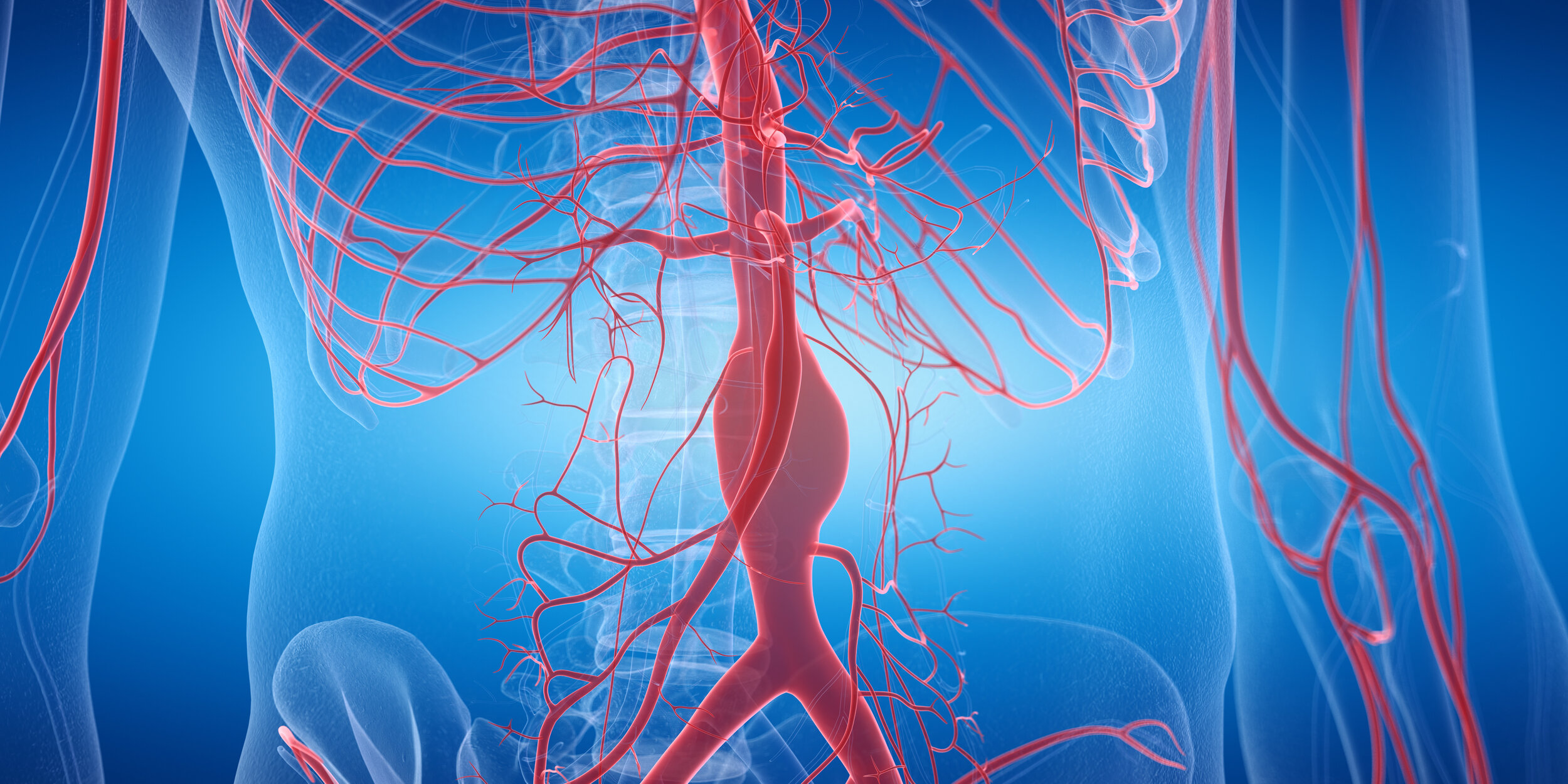
Aneurysms
An aneurysm occurs when the wall of an artery weakens and bulges, leading to the potential for a serious health risk. Aneurysms can occur anywhere in the body, most commonly in the upper and lower limbs, chest (thoracic aortic aneurysm) and abdomen (abdominal aortic aneurysm).
The aorta is the largest blood vessel in the body, running through the chest (thoracic aorta) and down through the abdomen (abdominal aorta). An aortic aneurysm occurs when the artery wall weakens and bulges, leading to the potential for a serious health risk. An aneurysm can gradually increase in size and the wall of the aorta will further weaken, leading to the risk of a rupture or dissection (tear) and cause life threatening bleeding.
Aortic aneurysms also place you at increased risk of blood clots which can break away and cause a stroke, as well as the formation of plaque (atherosclerosis) that can increase the risk of a rupture of dissection. The growth of an aneurysm must be monitored closely, and if intervention is necessary options include endovascular repair or open surgery.
Whilst aortic aneurysms can be symptomless, signs that you may have one include:
Pain in the jaw, neck or upper back
Tenderness or pain in the chest or back
Wheezing, coughing or shortness of breath as a result of pressure on the trachea (windpipe)
Hoarseness or difficulty swallowing
A burst or torn aneurysm can be a life-threatening medical condition. Seek immediate medical care if you notice any of the following symptoms:
A sharp, sudden pain in the upper back that radiates downward
Pain in your chest, jaw, neck or arms
Difficulty breathing
Carotid Artery Disease
The buildup of fatty plaques (atherosclerosis) in the arteries leading to the brain and heart (Carotid Arteries) is known as Carotid Artery Disease (CAD). There are many risk factors that can contribute to the occurrence of CAD, including but not limited to smoking, poor diet, age, high blood pressure and diabetes. Carotid Artery Disease can increase the risk of a stroke because of:
Reduced blood flow to the brain due to a massive build up of plaque
The rupture of a plaque, which can flow to a smaller artery in the brain. This can block the artery and therefore the blood flow to that part of the brain, causing a stroke
A blood clot where the plaque has formed and cracked. The clot can flow to a smaller artery in the brain and subsequently block the flow of blood to that part of the brain.
Atherosclerosis can occur in any artery within the body, and may not cause any signs or symptoms until a severe narrowing or blockage has occurred. Lifestyle changes, medicines and medical procedures can help to prevent or treat CAD and other forms of atherosclerosis, helping to reduce the risk of stroke.